Understanding Diabetes at the Cellular Level: The Story of Insulin Resistance ..
The Why of Diabetes... Much-Awaited Answer For Common People
GSHER DIABETES SUPPORT GROUP
11/14/20243 min read
Diabetes is one of the most common and complex diseases affecting millions worldwide. At its core, diabetes involves problems with the body’s ability to regulate blood sugar, also known as glucose. When we look closer, it’s clear that diabetes, especially type 2 diabetes, has a lot to do with how cells respond to a hormone called insulin. Here, we’ll break down how diabetes works at the cellular level and what insulin resistance means in simpler terms.
The Role of Insulin in Our Cells
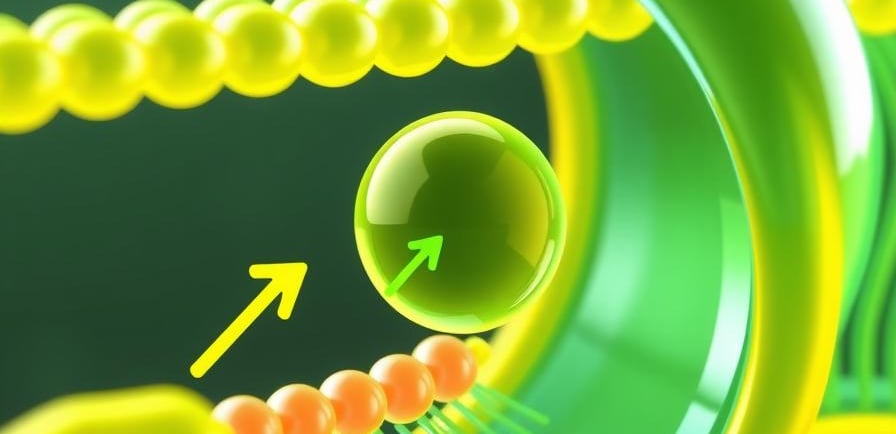
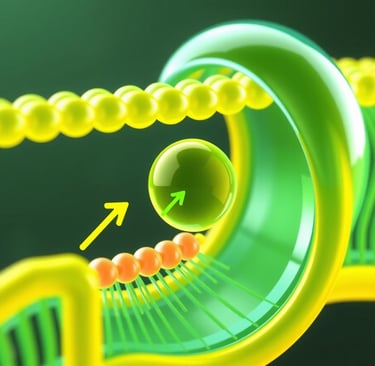
Think of insulin as a key that unlocks a door on the cell’s surface. This door allows glucose, a form of sugar from the foods we eat, to enter cells and be used for energy. When we consume carbohydrates (bread, rice, fruits, etc.), they break down into glucose in the bloodstream. Our body responds by releasing insulin from the pancreas. Insulin binds to receptors on cell surfaces, which signal “doors” on the cells to open up, allowing glucose to enter. This process is essential to keep blood sugar levels stable and give cells the fuel they need to function.
What is Insulin Resistance?
In people with type 2 diabetes, the “key” doesn’t work as well. Insulin binds to the receptors, but the cell doors don’t open as effectively, meaning glucose can't enter the cells easily. This condition is known as insulin resistance. With insulin resistance, cells become less responsive to insulin signals, causing glucose to build up in the bloodstream instead of entering the cells.
Why Do Cells Become Resistant to Insulin?
Several factors can contribute to insulin resistance. While genetics can play a role, lifestyle factors are also significant contributors:
1. High Levels of Fatty Acids: Excessive fat, particularly around abdominal organs, leads to the release of high levels of fatty acids in the blood. These fatty acids interfere with insulin signaling, making it harder for insulin to “unlock” the cell doors.
2. Inflammation: With increased fat deposits, the body releases inflammatory molecules. Chronic inflammation can alter insulin’s signaling pathway, leading cells to become less responsive to insulin over time.
3. Oxidative Stress: High levels of oxidative stress damage cells and disrupt insulin pathways, further contributing to insulin resistance.
The Cellular Mechanism Behind Insulin Resistance
At the molecular level, the cells in people with insulin resistance still have insulin receptors. But when insulin binds to these receptors, the signals that normally “open the doors” to glucose get interrupted. This disruption can happen in multiple ways:
Altered Receptor Function: The insulin receptors on cells may become less sensitive due to constant exposure to high insulin levels, similar to how our senses get desensitized to a constant smell or sound.
Blocked Signal Pathways: After insulin binds to its receptor, the signal it sends has to be relayed through a complex pathway to open glucose channels. In insulin resistance, parts of this signaling pathway are interrupted by molecules released by inflammation and fatty acids. This “interference” disrupts the signal, making it harder for cells to absorb glucose.
Fewer Glucose Transporters: Insulin signals certain molecules, known as glucose transporters, to move to the cell membrane and let glucose in. In insulin resistance, fewer of these transporters make it to the surface, reducing glucose entry into the cells.
The Body’s Response to Insulin Resistance
When cells don’t respond well to insulin, the pancreas tries to compensate by producing more insulin to help push glucose into the cells. This extra insulin may keep blood sugar levels normal for a while, but as insulin resistance worsens, even the additional insulin isn’t enough. Eventually, the pancreas gets overworked and can’t keep up, leading to higher blood sugar levels—this is when diabetes is usually diagnosed.
Can Insulin Resistance Be Reversed?
The good news is that insulin resistance can often be improved with lifestyle changes
Global Self-healthcare Education and Research (GSHER) is thrilled to announce the launch of our Diabetic Support Group, which is dedicated to empowering individuals in their journey to reverse diabetes through Therapeutic Lifestyle Changes (TLC).
Our support group offers:
Expert-led sessions on lifestyle modifications
Personalized guidance in therapeutic nutrition, exercise, and mindfulness- A supportive community to inspire and motivate positive change
Join us in embracing a path to better health and hope. Together, we can work towards reversing diabetes and enhancing quality of life.
Enroll today! Contact Swapnil at 8777011088 for more details.
GSHER Takeaway
Understanding insulin resistance at a cellular level shows how intricately our body responds to what we eat, our activity levels, and even our stress. Insulin resistance is like a rusty lock that needs attention. With lifestyle changes and sometimes medication, it’s possible to restore balance, reduce blood sugar levels, and improve overall health. Learning about these mechanisms empowers us to make choices that support our cells—and our well-being—for the long term.
Source: Dr Biswajit Mohapatra, Chairman
GSHER Support
Contact : Swapnil Mohapatra@8777011088
